The survey reports that dental caries (tooth decay) is the single most common chronic childhood disease in the country --5 times more common than asthma and 7 times more common than hay fever. Almost 50 percent of the 12 and the 15-year-old children have two teeth involved in the disease process. On the positive side more than 50% of the children between the ages of 12-15 years are caries free and on the negative side 97% of all carious lesions in these age groups are untreated. For the 35-44 year old group half of the lesions are untreated while in more than 90% of cases the treatment offered in extraction. The difference in caries experience for rural and urban areas is of particular interest. In rural areas, caries was found to be more prevalent in the surveys done in the past; similar higher levels of caries in the rural population were also noted in the present survey. The
data also shows that caries is very strongly age related and the average number of affected teeth goes up to almost 18 teeth per individual over the age of 65.
Most adults show signs of periodontal or gingival diseases. It is evident from the above data that periodontal health of the nation is very poor with only 28% of the 12 year olds having healthy gums and more than 93% of the 65 year olds have some gum or periodontal disease. These results indicate that periodontal disease including inflammation of gums and calculus is endemic in Pakistan. Like caries the level of gingival and periodontal disease is higher in the rural population of the country. Severe periodontal disease (measured as 6 millimetres of periodontal attachment loss) affects
about 17 percent of adults aged 65+. These data indicate that oral diseases are progressive and cumulative and become more complex over time.
The survey also showed that almost one percent of the 35-44 year olds and 20% of persons aged 65 years or above were edentulous (no teeth). Of the edentulous senior citizens more than one third had no dentures, while in the 35-44 year old group 35% required replacement of missing teeth and only 5% were wearing them. Chronic disabling diseases such as temporomandibular joint disorders affect 21% of the elderly and
compromise their oral health and functioning. The burden of oral problems is extensive and may be particularly severe in vulnerable populations like the rural poor. The public health capacity for addressing oral health is
dilute and not integrated with other public health programs. The public health infrastructure for oral health is insufficient to address the needs of disadvantaged groups, and the integration of oral and general health programs is lacking. Resources are limited in terms of personnel, equipment, and facilities available to support oral health programs.
There is also a lack of available trained public health practitioners knowledgeable about oral health. A national public health plan for oral health does not exist. This report presents data on access, utilization and financing of oral health care; provides additional data on the extent of the barriers; and points to the need for public-private partnerships in seeking solutions.
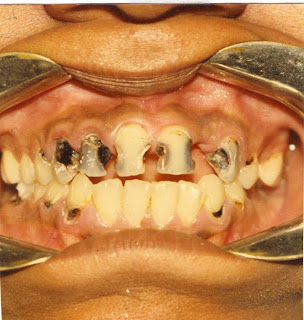
Oral diseases, particularly caries and periodontal disease, burden people in Pakistan excessively. Oral health has had low priority in the health activities of Pakistan, which has resulted in large unmet needs of the population and over 90% of all oral diseases remain untreated. From young adults to the 50 year olds lack of perception of their dental needs appears to be the most frequent reason for not going to the dentist. This lack of perception of needs, or ‘absence of toothache’, causes delays in seeking treatment and the
majority of patients present teeth at an advanced stage of decay which is usually beyond repair. One undesirable consequence of these delays is the observation that more than 90 % of all treatment given in the public dental clinics is tooth extractions. Moreover, preventive services (examination, scaling and prophylaxis) form less than 3 % of services at the public dental clinics and are testimony to the abysmal lack of oral health education,
preventive practices and the lack of dental health promotional programs in the country.
There is a paucity of data on oral health issues in Pakistan. The available data on dental caries prevalence show that Pakistan can be classified as a low caries country, on the positive side 50% of the children between the ages of 12-15 years are caries free and on the negative side 97% of all carious lesions are untreated (Maher 1991; Khan et al., 1990;
Khan 1992). There has been no pathfinder survey for the children since 1988 and no new published data on dental disease since 1992. Only one article on caries levels in the urban centers of Pakistan has been published in 2001 (Haleem & Khan 2001), which shows that this level has been static for more than a decade.
Khan et.al reported that 14-37% of 12 years old children had gingivitis and 11-37% of 15 years old had gingivitis whereas in both age groups 25-29% were with health gums.
There has, however, been no published data on the periodontal health of the nation since the last pathfinder survey of 1988.